Is H5N1 (Bird Flu) the Next Pandemic Causing Virus?
Everything you need to know about Highly Pathogenic Avian Influenza H5N1 (HPAI H5N1)
Influenza Virus Particles. Image Credit: Public domain/ Centers for Disease Control and Prevention/ Dr. F. A. Murphy, content provider/ 1973
Scientists are sounding the alarm about HPAI H5N1 (Highly Pathogenic Avian Influenza H5N1, referred to in this article as H5N1) and it’s potential to be the next pandemic causing virus. Recent human infections have indicated H5N1 has been acquiring mutations that improve it’s ability to infect people.
One critical aspect of H5N1 becoming a pandemic causing virus is developing person to person transmission, this has not yet been reported for the virus. However, research published December 2nd, 2024 in Nature Microbiology makes a strong case for increased virus shedding and hence airborne transmission being a key component of increased infectivity. The researchers found that increased viral shedding in H5N1 found in an infected dairy farm worker but not in H5N1 that infected the in cattle themselves. This means the virus in that person had changed in a way that allowed for improved airborne spread. This supports prior research published October 28th, 2024 in Nature showing that the same virus strain (A/Texas/37/2024 (huTX37-H5N1) had acquired a mutation that improved the virus’s ability to infect human cells and increased lethality in animal models.
Repeat human infection gives the influenza virus more chances to develop mutations. Within the last month several reports have indicated that H5N1 is moving closer to person to person transmission while maintaining it’s highly pathogenic nature, exactly what we don’t want.
I have gotten hundreds of questions on social media about this so I will start with some of the basics to help everyone navigate what might be coming next. Let’s dive into where H5N1 came from, why is it more concerning than annual influenza strains, and what can we do to protect ourselves?
What is H5N1 and where did it come from?
Highly Pathogenic Avian Influenza (HPAI) H5N1 has been making steady headlines since the dairy farm outbreaks began in the summer of 2024 (first detected in cattle in March of 2024), and most people may have heard about it in passing as one of the reasons egg prices continue to rise. H5N1 has been detected in over 110 million birds (wild, backyard flocks, and commercial poultry operations) in 49 states since 2022.
Although scientists have been tracking H5N1 for nearly six decades with it’s first isolation in Scotland in 1959. However, it is now fast-tracked towards becoming person to person transmissible which could start another global pandemic.
Charostad, J. et al. Travel Medicine and Infectious Disease 2023
The direct precursor to the H5N1 that we are contending with today was first detected in a goose farm in Guangdong, China in 1996. This was quickly followed by a small outbreak of H5N1 in Hong Kong in 1997 where the crude fatality rate was 33%. The spread started with sporadic human cases, the first two reported being more than 6 months apart in China, but as more wild birds and subsequently bird flocks in close contact with people began to fall ill, more human cases were recorded. In data spanning the years 2003 to 2023 the WHO recorded 878 human cases in 23 countries with a fatality rate of 52%.
Recently, (2022) the virus was detected in wild mammals in the United States followed shortly by detection in wild mammals in Canada, Japan, China, and most of Europe, Virus adaptation to infect mammals is a crucial step towards human to human transmission. It has also remained highly pathogenic (high mortality) as it mutated to infect mammals. H5N1 caused mass death in populations of communal marine mammals (seals and dolphins), and terrestrial mammals such as foxes, bobcats, bears and mountain lions. H5N1 has been detected in wild mammals across the United States.
Source page: Detections of Highly Pathogenic Avian Influenza in Mammals, last updated 2024, USDA. Link to USDA website here.
In 2023 it was reported that sequencing of human infections of H5N1 has shown (genetic variation and divergence from H5N1 circulating in wild bird populations, indeed genetic divergence in human cases is being seen across the globe. What this means is that the widespread nature of the virus is leading to more human infections and therefore more attempts or chances for the virus to hit the right combination of mutations that enable person to person spread.
This is a bit simplified, but, recent news of infection in swine and the hospitalization of a teenager with no underlying conditions in the ICU in British Columbia, Canada are signals to scientists that we are getting closer to viral adaptations that will allow for to person to person spread while the virus may retain its high pathogenicity (mortality rate).
However, it’s not all bad news. We likely have some protection from this year’s and previous influenza vaccines. Let’s go over some of the basics.
What do H and N stand for?
To provide a way to understand how mutations, prior infection, vaccines might hurt or help, let’s quickly review some of the basics. H stands for Hemagglutinin and N stands for Neuraminidase, these are two proteins on the surface of an influenza virus and they organized by number.
Image credit: https://pubs.rsc.org/en/content/articlehtml/2021/ra/d0ra07283d
For example, there is H1N1 where the H is different but the N falls into the same classification as the one found in H5N1. Our immune system can recognize these proteins and make antibodies against them to stop infection, or identify infected cells as part of an effector T cell response.
Now it gets a little trickier, because the N in H5N1 is most often found with H5 it may have mutations that it picks up, making it distinct from the N found in H1N1 even though there are more closely related than the N2 found in H3N2 influenza.
When two different strains of influenza infect the same person or animal they can undergo reassortment where they may exchange the genes for H and N leading to different combinations of H1, H2, H3-H18 and N1, N2, N3-N11 numbers. Reassortment is different than how SARS-CoV-2 viruses can mix their genetic information during co-infection. SARS-CoV-2 can undergo recombination, swapping genetic material during co-infection along the length of the virus which sometimes leads to nonfunctional combinations.
Our immune systems can recognize the H and the N separately which means an H1N1 vaccine, like what is found in this year’s flu shot can offer some protection (though not as good as a perfectly matched vaccine). Also, because of the mutational drift of certain N1s evolving separately (H5N1 and H1N1) the immune system may not have perfect recognition of these different N1s.
Why Are Scientists and Doctors More Worried About H5N1 Than Other Influenza Viruses?
The reason why this version of H5N1 avian flu is called highly pathogenic is that it has a very high death rate in infected animals and people. With a case fatality rate of over 50% in people, H5N1 sounds terrifying. However, this death rate is likely to come down significantly. Often initial cases only represent the most critically ill people who may not have immediate access to medical care, but sought it out only after severe illness developed. This may inflate mortality rates as people who recover are not counted in numbers of infected people. For example, early death rates during the SARS-CoV-2 pandemic were much higher initially.
Seasonal influenza has an population average case fatality rate ranging from about 0.12% (1.2 per 1,000 infections) which roughly doubles every 5 years after the age of 65, peaking around 4.3% at 85+ according to one Dutch study, and is currently the 12th leading cause of death in the United States.
So why are scientists so concerned? Highly pathogenic influenza viruses, such the H1N1 that caused the 1918-1919 pandemic (Spanish Flu) can have significantly higher death rates than a typical influenza season. For example, the 1918-1919 pandemic had an estimated case fatality rate of >2.5% about 25-times higher than a typical ~0.1% case fatality rate across an entire population. Therefore, even if death rates drop to about 2.5% as many as 130,000 to 1 million people in the United States (depending on how pathogenic the virus is) could die in a single influenza season which typically lasts 4-5 months. This is why scientists are concerned. With no prior immunity death rates could be higher than those seen at the peak of the COVID-19 pandemic, possibly more. However, I believe it is unlikely that death rates will be this high. Let’s go over why next.
Will This Year’s Flu Shot Help?
H1N1 is present in this year’s flu shot and has been present in the seasonal influenza shot for several years. Therefore, for everyone who has had a flu shot in recent years your immune system has been exposed to the N1 protein and although it may not be a perfect match to the N1 in H5N1 some immunity may be protective from the most severe disease.
Prior exposure to H1N1 has been shown to be protective in animal models. In one study using ferrets (a common model for human influenza) prior vaccination with H1N1 reduced illness and death in ferrets infected with an otherwise lethal dose of H5N1. Though the animals were still infected they did not have severe disease and none of the animals in the vaccinated study group died. In another study looking at ferrets, the authors showed that H1N1 imprinting provides complete protection against H5N1. In a third study antibodies from people previously infected with H1N1 transferred to mice. These antibodies were highly protective from H5N1 infection in the mice. The same antibodies were able to neutralize H5N1 in vitro (in a dish). This study from Chen, Y-Q et al. also encourages examination of vaccine formulations to promote stronger responses to the Neuraminidase protein.
So what does this research tell us? On average, adults in the United States are infected with influenza about once every five to seven years meaning most people, unless you have gotten your annual flu shot, you are unlikely to have high numbers of circulating antibodies. Flu shots from previous years and confirmed infection with a N1 containing influenza variant may provide some memory protection though it is unlikely to protect from initial infection, spread of the virus, and protection against severe disease is not guaranteed. Protection against severe disease is not guaranteed for a few reasons. As time goes on the immune system doesn’t remember the prior pathogen as well, the mutational drift may make it look different, as we age the immune system declines in function. Finally, as SARS-CoV-2 infection can cause immune system dysfunction particularly with IFN-y production a key cytokine in fighting the influenza virus, which may lead to more severe infection.
However, due to routine vaccination and previous H1N1 exposure most of the population is likely to have less severe disease, on average. But, influenza can still be deadly for those in vulnerable populations and infants too young to get an influenza vaccine. Again, a confounding factor with as of yet uncharacterized impact in these predictions will be the toll that COVID-19 can take on immune system function, which may leave more of the population vulnerable to severe viral infections.
How Close Are We To H5N1 Becoming A Pandemic Causing Virus?
In order for H5N1 to become a highly pathogenic pandemic causing virus it must do two things:
H5N1 must adapt through mutation to enable effective person to person transmission.
After gaining the ability to spread between people, H5N1 has to retain its highly pathogenic nature. Sometimes when viruses mutate they lose their deadly characteristics, but this doesn’t appear to be happening with H5N1 so far.
As of this writing (Dec. 3rd, 2024), H5N1 outbreaks have been reported in 689 dairy herds across 15 US states. Some dairy farm workers have developed H5N1 infection which so far has manifested as mild infection characterized by conjunctivitis (pink eye), in a few cases this has developed into a respiratory infection. The virus sequenced from these infection has until recently, has not been well adapted to human infection which is likely why the infection was mild. However, a teenager with no underlying conditions was admitted into an ICU in British Columbia, Canada with severe respiratory illness. The H5N1 virus sequenced from the teenager is distinct from the version of the virus circulating in US dairy herds and also distinct from H5N1 found in local bird flocks, and had also acquired two mutations that improved it’s ability to infect human cells. As no source has been identified this has led scientists to hypothesize that there is a different intermediary source that has yet to be identified. What this looks like in the viral evolution game is another loud ‘knock on the door’ as the virus moves towards effective human to human spread.
In California a child was recently confirmed to have H5N1, but the illness was mild, resolved on it’s own, and was not spread to family members. As of the time of this writing no confirmed source of infection has been found, however H5N1 has been found in raw milk for sale in California, sales of raw milk in the state have been suspended.
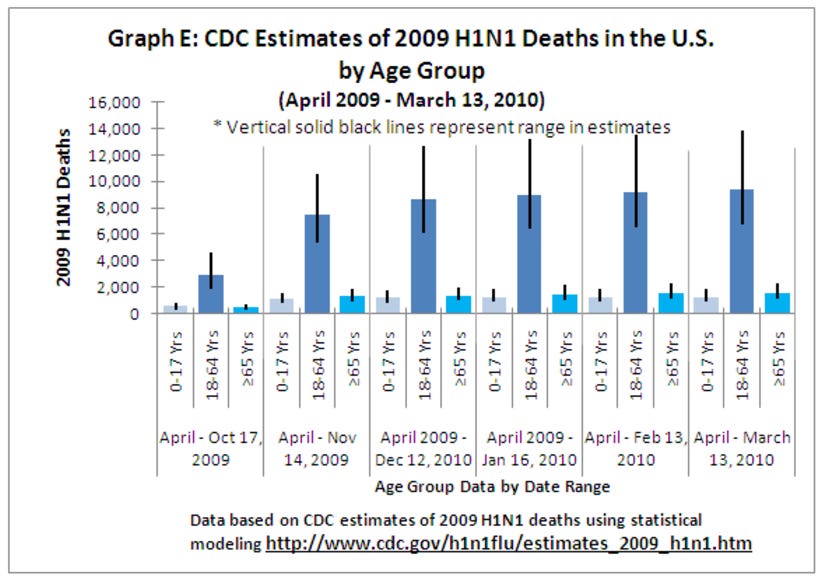
Finally, a pig at a small farm in Oregon died from confirmed H5N1 infection. This is significant because pigs have cell surface molecules similar to those in humans that influenza can use to infect a cell. Influenza can gain critical adaptations in swine populations that allow it to better spread between people. This is why many influenza outbreaks start in pigs, for example, the 2009 swine flu pandemic which caused an estimated 284,000 excess deaths world wide. In the United States where an estimated 72-81 million people were vaccinated (despite delayed vaccine roll out) there were about 60 million cases, 270,000 hospitalizations, and 12,270 deaths. However, it was unusual that people between the ages of 18-64 years old had the highest death rates, similar to the W-shaped mortality curve of the 1918-19 pandemic.
Although, person to person transmission has yet to be documented, the findings above are a signal to scientists that the zoonotic leap is not too far away. Given the increase in infections in people as well as animals such as pigs that often serve as zoonotic vectors for influenza, I expect the virus to adapt to person to person spread sometime within the next two years. I’m actually hoping this estimation of the timeline doesn’t age well (I’d rather not have H5N1 circulating in the human population ever), but I do hope this estimate serves to help people think about ways to be prepared.
Update December 27th, 2024: I am updating this article to include a recent publication and the new genetic sequencing data from two H5N1 cases. In Louisiana, United States a 65 year old man was hospitalized, and as mentioned above a teenager in British Columbia, Canada was hospitalized. In these two separate cases mutations were found that would enable human to human transmission of the virus. As of this writing no human to human transmission has been identified.
So, How Bad Will It Be?
When H5N1 adapts to person to person spread it is unlikely to be as devastating as SARS-CoV-2 was in the United States for the following reasons:
The United States has a influenza vaccine and infection experienced population against one of the variants of N1, this is likely to reduce disease severity and death rates on average.
Hygiene (hand washing) and proper mask wearing learned during the SARS-CoV-2 pandemic will help slow virus spread and reduce infection and/or severity of infection in those that practice these healthy habits.
mRNA based vaccine technology will enable rapid ramp-up of H5N1 vaccines to meet demand once the virus begins to spread person to person.
In short, I expect there could be intermittent school closures in areas hardest hit by outbreaks and there might be some measures similar to those taken at the beginning of the SARS-CoV-2 pandemic. However, I expect far fewer hospitalizations and a lower death rate than COVID-19. Also, influenza has a significantly lower reproductive rate (Re also known as Ro or R-naught) than SARS-CoV-2 meaning that the spread will be slower making it easier to contain outbreaks.
One issue that is a wild card is how much COVID-19 induced immune system dysfunction and dysregulation may contribute to more severe disease. Another issue is pandemic fatigue. Many people have become fatigued regarding recommendations to maintain personal cleanliness (hand washing) and protecting themselves (mask wearing). It is difficult to predict the contribution of these two factors, but I anticipate a measurable impact. Those who have recently had SARS-CoV-2 should, in my personal opinion, be vigilant about avoiding H5N1 when person to person transmission begins.
Like most viruses the simple acts of masking, washing your hands, and staying up to date with vaccines will go a long way to protect you and your loved ones from H5N1.







Wonderfully informative, as always. Thank you!