Long COVID Series Part 4.3: Is there evidence for a link between Cancer and COVID-19?
Because SARS-CoV-2 disrupts immune system function, which is important for fighting off cancer this review is under the umbrella of SARS-CoV-2 and the immune system (Part 4).
Cancer
Cancer is one of the most frightening words in the English language. It is a disease that shows up seemingly out of the blue, upends our lives, sometimes taking our loved ones away from us in mere weeks.
Given the immune system dysfunction, long-lived nature of infection, and chronic issues caused by SARS-CoV-2 infection, it’s logical for cancer biologists and immunologists to ask if increased cancer rates is the next ‘shoe to drop’ in the aftermath of the COVID-19 pandemic.
Early detection is still the best way to increase chances of cancer survival, and cancer immunotherapies have made some cancers survivable, extending life for millions. However, as rates continue to rise and age of first diagnosis has continued to drop in the United States, many researchers are asking, why?
The answer is unfortunately not straight forward. Cancer can be linked to several different causes, including; chronic toxin exposure, weight, poor diet, lack of exercise, extreme chronic stress, genetics, and viral infection.
Viral infection is a leading cause of cancer, causing up to 1 in 5 cancer deaths. This rate is only surpassed by tobacco use which causes about 20% of all cancers and 30% of cancer deaths in the United States. Viruses such as human papillomavirus, hepatitis B virus, Epstein-Barr virus, and human T cell leukemia-lymphoma virus (HTLV-1) are estimated to cause 15% to 20% of cancer cases worldwide (Hausen, H. et al Science 1991, The 7 Viruses That Cause Human Cancers, American Society for Microbiology, 2019).
A success story of reducing cancer through vaccination is the story of Human Papilloma Virus (HPV) and the six different types of cancer attributed to HPV infection. HPV infects ~80% of adults and the HPV vaccine is credited with stopping nearly 90% of cancers caused by the virus. In a 2020 study of 1.67 million women and girls HPV vaccination reduced the risk of invasive cervical cancer by 88%. This highlights the virus-vaccine-cancer prevention axis in stark relief.
So, how do viruses cause cancer?
There are two big ways: 1) Chronic infection and/or disruption of normal cellular activities which can lead to persistence of mutated cells, and 2) Immunosuppression.
A common feature between the viruses discussed in the introduction is that the human immune system fails to clear the virus and the person is typically infected for life. This allows a virus to continually disrupt cell and immune system function, and eventually something may break, often in the form of cancerous cell development. For example, the immune system is always looking for virus infected cells or cancerous cells to eliminate. Viruses employ several mechanisms by which they hide from the cells of the immune system when they take over one of our cells. This becomes dangerous during chronic viral infection. At a high-level, while replicating inside one of our cells mutations can eventually leads to ‘transformation’ of these cells into cancer cells that are hidden from the immune system. As for immunosuppression, we know that the rate of cancer is higher in people infected with a virus that suppresses the immune system, such as HIV. When someone is immunocompromised this disrupts the immune system’s ability to seek out and destroy cancerous cells, increasing the likelihood of developing cancer.
To read more about the history of and relationship between viruses and cancer follow this link.
Cancer and COVID-19
To be abundantly clear, at the time of this writing I do not believe there is definitive evidence linking SARS-CoV-2 infection to the development of cancer.
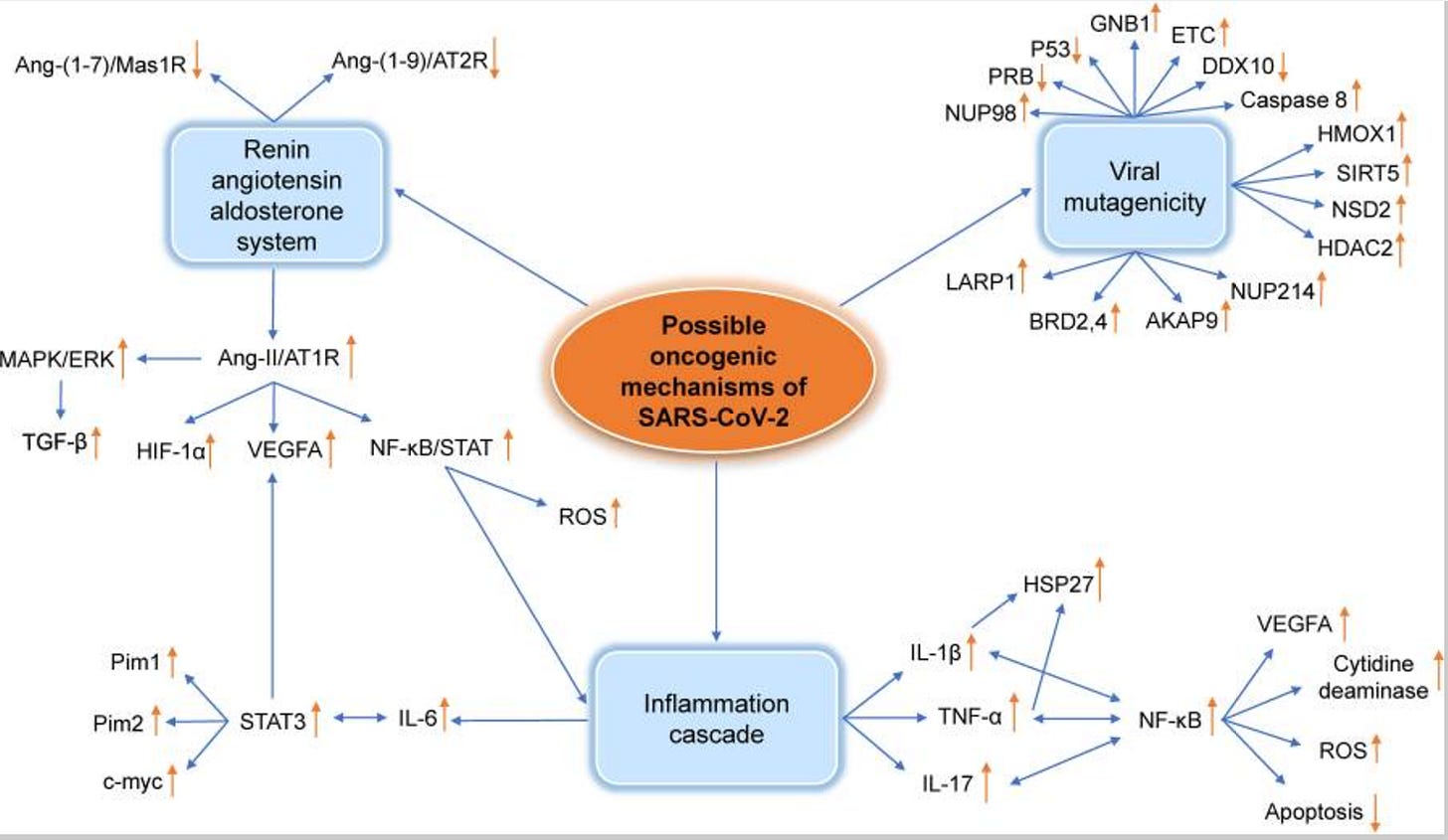
The SARS-CoV-2 virus however boasts activity that is aligned with the two primary ways that viruses are linked to the development of cancer: 1) long-lived residence in tissues, and 2) disruption of normal immune system function and immunosuppression. Additionally, several oncogenic factors are increased by SARS-CoV-2 infection (see pathways below). Cancer and changes in rates of cancer can take years to show up in a population. Additionally, the lack of screening during periods of lockdown lead to an increase in the diagnosis of advanced cancers which could mask an increase in overall incidence for a few years.
Link to reference can be found here: Jahankhani, K. et al, 2023
Indeed, a potential link has been hypothesized both by scientists and physicians, but a link has yet to be established, and I believe it will be a few more years of research before one could be identified. What we have for now are research studies that indicate certain known proteins and pathways are triggered by infection with SARS-CoV-2, a few early studies, and physician reported observations.
Let’s go through some examples of each.
First, a predictive study analyzing genes upregulated in a host of viral infections found that the most probable malignancy to occur after infection with SARS-CoV or SARS-CoV-2 was pancreatic adenocarcinoma (Pancreatic cancer). The authors do cite real world evidence of changes in pancreatic morphology and injury post-COVID-19. However it is important to remember that gene upregulation and overlap does not necessarily guarantee cancer development and more observational work will need to be done to confirm the in silico (predictive) findings.
Next, a genome-wide association study examining COVID-19 and Lymphoma data sets found that COVID-19 patients with severe respiratory symptoms have an increased risk of developing diffuse large B-cell lymphoma (p = 0.006 for my scientist friends). The authors did not identify an increase in risk for Hodgkin’s lymphoma or other types of non-Hodgkin’s lymphoma. Finally, the authors conclude that severe COVID-19 ‘may’ be a risk factor and I agree with the authors that follow-up studies and larger sample sizes are needed. However, this link would not be especially surprising as some diffuse large B-cell lymphomas have been linked to viral infection and chronic immune system stimulation. Review linked here: Gergely, L. 2024.
Another possible clue as to a potential mechanism by which SARS-CoV-2 could induce cancer is the observation that the tumor suppressor gene p53 is down-regulated for at least 24 weeks after infection in patients suffering from long COVID. Over 50% of all human cancers have disrupted p53 activity either through mutation or via proxy by pathway disruption. It is important to remeber that other viral infections such as Influenza and Herpes viruses can disrupt p53 activity (by increasing it), but in the case of Influenza which is not linked to cancer I was unable to find evidence that this disruption is long-lived. Again, I agree with the authors that: “A causal relationship between SAR-CoV-2 and cancer has not been demonstrated but, if confirmed, it would have enormous impact on public health.” This is why I am providing an overview of some of the evidence despite there being a lack of a definitive link.
A 2023 study (Dugerdil, A. et al.) looked at the question in reverse and hypothesized that severe SARS-CoV-2 could serve as a marker for undiagnosed cancer. Their findings showed that a total of 897 of the 41,302 (2.2%) of people admitted to the ICU with SARS-CoV-2 infection were diagnosed with cancer during the follow-up months as compared to 10,944 of the 713,670 (1.5%) of controls who were diagnosed with cancer. In this study the individuals who had been admitted to the ICU had a 1.31 times higher risk of a cancer than those who did not require hospitalization for SARS-CoV-2 infection. When analyzing larger data sets the team found a higher risk in diagnosis of renal, hematological, colon, and lung cancers. The patient follow-up period in which a new cancer diagnosis was identified was between 22.5 and 4 months after admission to the ICU. I am in full agreement with the authors that this does not indicate a clear cause and effect relationship, but the data does indicate an increased risk of cancer diagnosis post-ICU admission for SARS-CoV-2. If it’s an indicator of an underlying cancer or a causative agent remains to be determined.
Given the magnitude of a potential health crisis if SARS-CoV-2 is determined to be an oncogenic virus I think it is important to share the words of patient facing physicians who also rightly claim that they can not produce a definitive association, but they have noticed an increase in what they called ‘unusual’ cancers. In June of 2024 The Washington Post published an interview with several scientists and physicians on this topic. Among them was Dr. Kashyap Patel who details his concerns regarding suddenly seeing an increase in cancers that are typically found in patients in their 70s and 80s, in people decades younger. He has teamed up with scientists who have also noticed a trend in increased expression of cancer markers after SARS-CoV-2 infection and the investigations into this are presumably still ongoing. However, I would like to echo what the interviewees themselves said “I hope we’re wrong”. The health implications of being right are enormous.
The full article by Ariana Eunjung Cha can be found here: ‘Unusual’ cancers emerged after the pandemic. Doctors ask if covid is to blame.” More about the types of cancers and potential causes that Dr. Patel is seeing can be found here: Kashyap Patel, MD, Sees Link Between COVID-19 and Cancer Progression, Calls for More Biomarker Testing
Summary
There are additional breadcrumbs in the literature and anecdotal notes from practicing physicians, however nothing is tantamount to a smoking gun that links SARS-CoV-2 infection to cancer. I would like to caution the reader that this doesn’t mean that there isn’t a link, just that good research on slowly progressing diseases can take a lot of time to do right. Typically scientifically accepted links are established by a body of literature and observations, not a single study. My personal view is that SARS-CoV-2 is linked to so many other physical issues, ones that can also cause an enormous amount of stress on the body (which can also cause cancer) and long-term health issues, that it is better to avoid infection and maintain recent vaccination status to reduce the potential impact of a breakthrough infection.
Though often managed better with the novel therapeutics developed in the last couple of decades, cancer remains the second leading cause of death in the United States. As of this writing (January 2025) the final totals of new cancer diagnosis are being tabulated for 2024 and are expected to exceed 2 million new cases. This is a record number for the United States, impacting more than 1 in 200 people in our entire population in just one year. Therefore, I hope this article also serves as an important reminder that early diagnosis, minimizing activities associated with cancer development, while introducing healthy habits in 2025 can go a long way.
Subscribe and join me for the next part of my series on Long-COVID where I will tackle the topic of The Neurological Impacts of Long COVID which will cover both central nervous system (brain) and the peripheral nervous system which includes everything from blood pressure and cardiac function.






I am concerned with how the next few years will look. We are understanding that infections are becoming more problematic than we initially thought.