My Rapid COVID-19 Test is Negative... but...
We're in a virus 'shoulder season', so which virus did you get?
SARS-CoV-2 is without a doubt on the rise in the United States with COVID-19 hospitalization increasing 19% over the last 14 days. Kansas, Vermont, Georgia, and Rhode Island have had over a 90% increase in hospitalizations in the last 14 days (per US Dept. of Health and Human Services). However, there are a lot of other viruses in circulation, such as Rotavirus (mostly dangerous for infants and young children, transmission route is fecal-oral), which has boasted just under 25% positivity rate over the last three weeks.
Typically, the transition from summer to fall is a period of prominent virus ‘change over’ with viruses that typically spread well in the summer months decreasing and viruses that tend to spread better in winter months starting to increase. Hence, we’re in a ‘shoulder season’ without any one virus claiming complete dominance in infection rates.
Graphic representation of 10 human viruses (creative common licence figures from VIPERdb https://viperdb.scripps.edu (Carrillo-Tripp et al. 2009) and Reddy et al. 2015). The virus families included here are: a Picornaviridae, b Coronaviridae, c Caliciviridae, d Astroviridae, e Togaviridae, f Bunyaviridae, g Rhadoviridae, h Filoviridae, i Orthomyxoviridae, and j Paramyxoviridae.
Although SARS-CoV-2 can spread in the heat of the summer, it typically surges during late December though early January. In the last few years cases have started to rise after the 4th of July, just as they have this year.
If you’re feeling under the weather and are coming up negative on multiple COVID tests, without a PCR test it is hard to be sure, but it is possible you have a completely different virus. We have all been hyper focused on COVID, with good reason, but as we move into the fall there’s still a chance that you may not have COVID at all.
So, which ‘bug’ could it be? Below are some of the most common viruses we encounter that can cause severe disease.
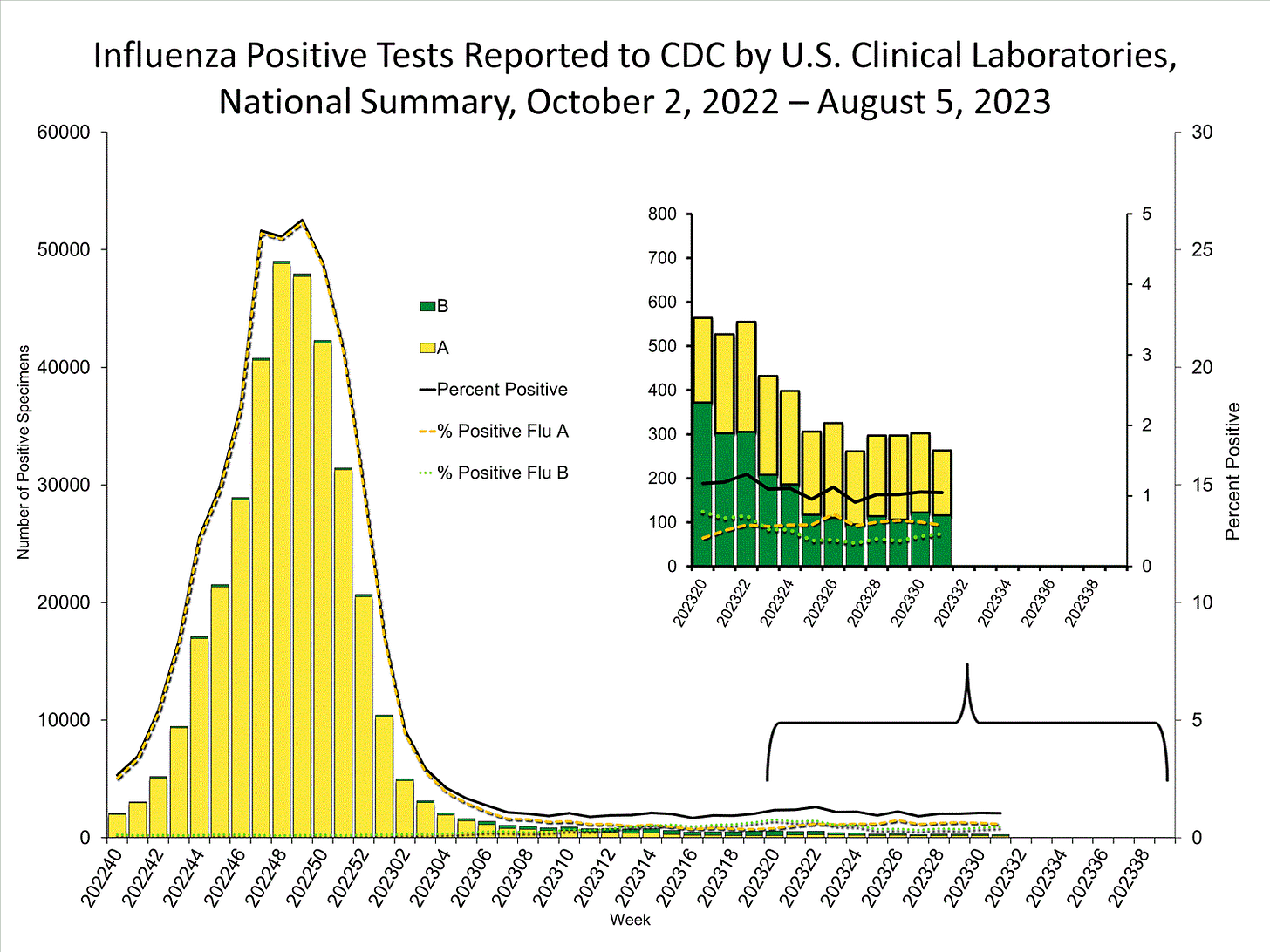
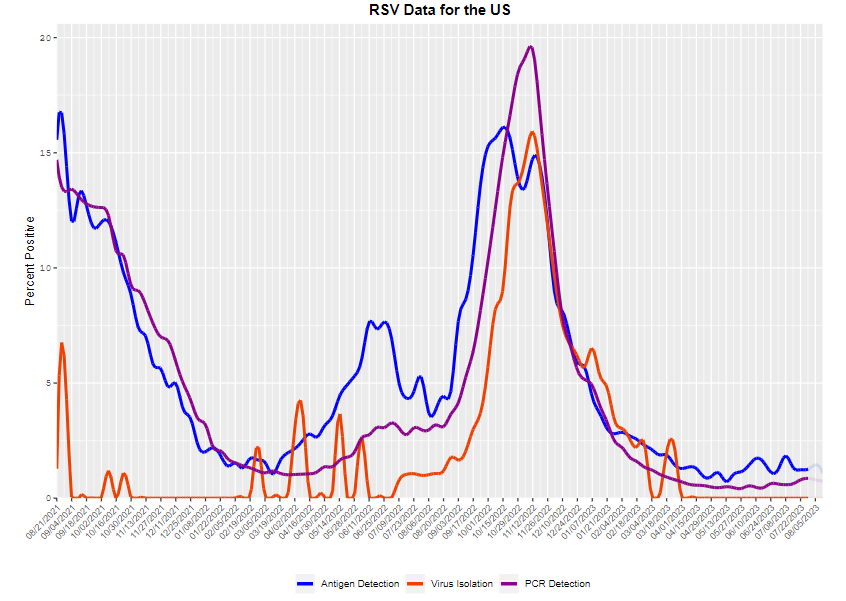
Note, the graphs taken from the CDC showing virus prevalence across the United States (data current as of 8/16/2023). The linked titles will take you to each page where you can explore levels in your area and read about typical symptoms.
Even if you are coming up negative on a COVID-19 test, do not hesitate to contact your medical provider for advice if you have severe symptoms and wear a mask out and about because: 1) Spreading other viruses can be deadly to others too, and 2) co-infection with SARS-CoV-2 and another virus could land you in the hospital.
In the next few months we can expect COVID-19 and Influenza to continue/begin to increase. Last year was an unusual year for RSV and I am hesitant to make predictions re: behavior of this virus, though it is likely to rise with the start of school.
Vaccines for Influenza and an updated COVID booster will be available this fall. RSV vaccines for 60+ have been approved by the FDA. Do note that the FDA has asked for continued data monitoring for Guillain-Barre syndrome, please discus the risk-benefit with your primary care provider. For babies and children up to 24 months the FDA has approved a monoclonal antibody (Beyfortus) to protect from RSV infection. RSV can be dangerous in infants and reducing RSV infection early in life reduces the chances of developing asthma later in life.
SARS-CoV-2: Intermediate and Rising
Weekly hospitalization data (blue) and weekly deaths (orange) per CDC, 8/16/2023 (below).
Weekly hospitalization data (blue) and weekly positivity data (orange) per CDC, 8/16/2023 (below).
Human Parainfluenza Virus Types 1, 2, & 3: HIGH, HIGH, & LOW
Respiratory Adenovirus: LOW (Decreasing since mid-June)













Thank you for this. Thank you for all you do to get information to people. You have saved the health of many. We need more people like you.
This is a question from a COVID cautious retired nurse “Dire. I don't understand how this specific SARS virus is able to have so many variants. Do you know? It is the one fact, I don't understand.”
For those who have the genotype which means they are assymptomatic if infected, is it known if they can still get serious health problems from COVID? Brain, vascular, oran damage? Are they at less risk? Or will they just not see the freight train coming? An elderly neighbour with health issues is taking risks, while saying she has still not had COVID. No mask. A friend who has really been following COVID and active in getting knowledge to others is not masking at times when there is absolutely risk! Also not fit testing mask. Makes me sad.