Which Arm Should You Get Your COVID-19 Booster In?
It sounds strange but it really might make a difference, here is why....
In case you can’t remember which arm you had your last COVID-19 booster in (I couldn’t) just remember that most people giving vaccines tend to give it in the recipient’s non-dominant arm. This reminded me that, yes, 10 months ago or so, it was in my left arm.
But does the arm it is given in matter? According an article in Lancet eBioMedicine Differences in SARS-CoV-2 specific humoral and cellular immune responses after contralateral and ipsilateral COVID-19 vaccination, Ziegler et al. 2023, it may. The reason I say it “may” is that replication in human studies is important before claiming something has a definitive benefit, but their study results seem relatively solid for a small population.
Notably this study only reviewed responses from “naïve” individuals (ie they did not have COVID infection). Since COVID infection is systemic it may not matter as much if people have both had COVID and been vaccinated, but also it certainly couldn’t hurt to choose the same arm for vaccination.
Let’s review.
The study included a total of 147 people received their second Pfizer COVID vaccine in the same arm and 156 received in the opposite arm. Two weeks after the second shot IgG antibodies that bound the spike protein, the strength with which they bound, and if they could neutralize the virus was examined. Also spike protein specific T cells (CD4 and CD8) were analyzed.
What was the same between the two groups?
Median spike-specific antibody IgG levels were not different
IgG binding strength to the spike protein was not different
Cytokine levels were not different
Adverse events were not different
What was different between the two groups?
Neutralizing antibody activity was significantly higher in people who received their second shot in the same arm.
CD8+ T cells that were antigen specific were higher in people who received their second shot in the same arm.
CD4+ T cells were the same, but people who received their second shot in the same arm had antigen specific CD4+ T cells that had less of the exhaustion / tolerance marker CTLA-4.
It is important to know that infection outcomes were not included in this study, however there is strong evidence in multiple research studies linking higher amounts of neutralizing antibody to better overall protection from initial infection and improved infection outcomes.
Is there an Immunological explanation for this?
When new findings like this are published, I first ask is there a biological or Immunological basis for something like this occurring? For example, there is no clear mechanism of action for how Ivermectin could impact COVID-19 infections and over the last several years no one has delineated one, but there is a trail of expensive failed clinical trials. But there is logical support for the findings that vaccination in the same arm could be beneficial.
First, it is important to understand that we have lymph nodes all over our bodies. Lymph Nodes are dime to silver dollar sized nodular structures where immune cells (white blood cells) gather to share information about foreign invaders.
(Image Credit: Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014")
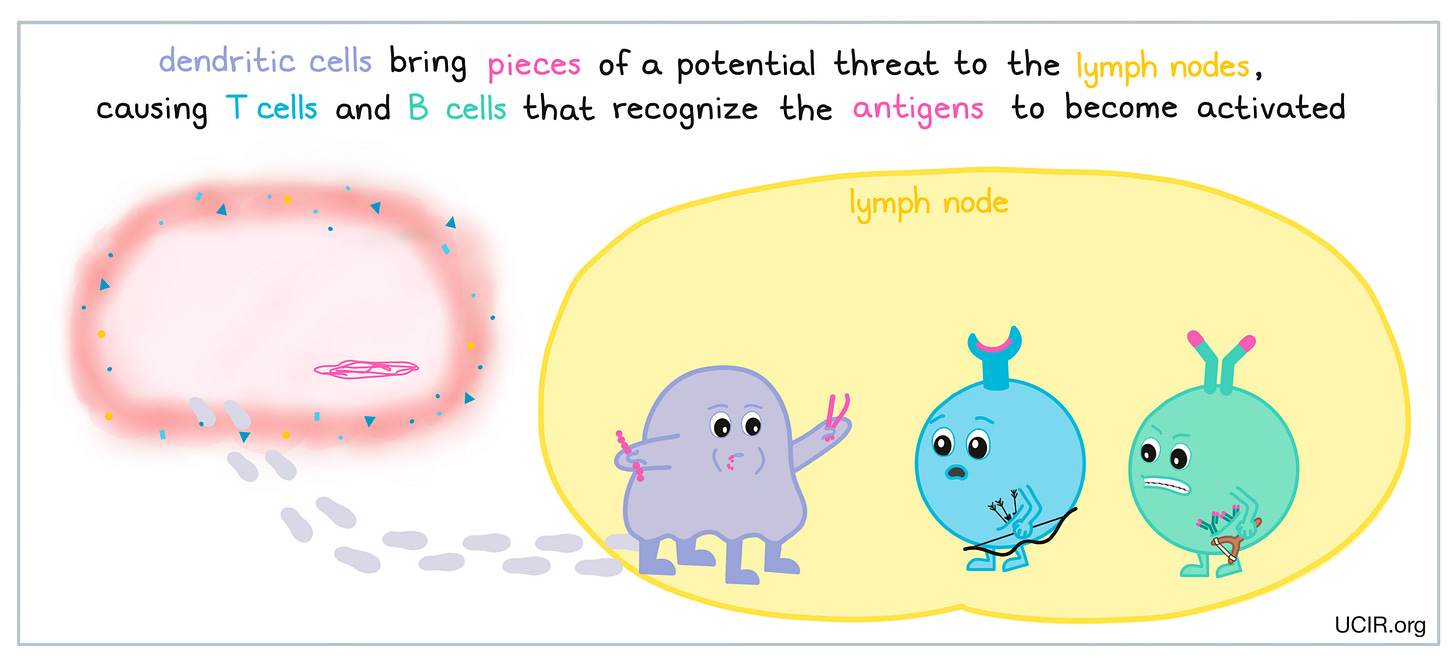
One of my favorite professors liked to say it’s the bar where everyone goes to meet and gossip. This is true, when inflammation occurs, white blood cells enter the affected lymph node quickly, causing it to swell up. When you receive a vaccine in your arm, the antigen in the vaccine travels to the nearest draining lymph node, typically the axillary lymph nodes located roughly around the base of the armpit on the same side. This is where the immune response will start.
(Image Credit: https://www.ucir.org/immunology-101/getting_to_know_the_immune_system)
Once the infection is gone, or the response to the vaccine is over, most people have memory cells that remember signatures of the pathogen and can respond quickly the next time they encounter those specific signatures. These are pathogen specific T and B cells that are very long-lived and can help fight off infections in the future. The development of memory cells is a hallmark of the adaptive immune response.
So, why the same arm? Well, there is evidence that memory B cells may persist not only in the bone marrow (they usually head back there and live for years to decades) but that they spend a long time in the draining lymph node, or lymph node where the primary vaccine or pathogen response occurred. Here is one publication detailing this phenomena in mice: Recruitment of memory B cells to lymph nodes remote from the site of immunization requires an inflammatory stimulus. This was done only in mice because whole lymph node responses are difficult to study in humans, as we don’t typically remove lymph nodes unless there is severe disease. But this study showed that when the antigen shows up again (in this study in the form of a vaccine) the memory B cells are already there and ready to respond and divide some more. It is highly likely the same mechanism for rapid pathogen response is maintained in humans.
But what if it is a different antigen or spike protein?
We know our boosters this fall are going to be based on XBB.1.5, but we also know that human B cells can continually adapt, the do not have evolutionary dead-ends like the hypothesis of original antigenic sin proposes. And, yes, we have real world evidence for this (here is a fantastic paper on it that is Sars-CoV-2 specific: Increased memory B cell potency and breadth after a SARS-CoV-2 mRNA boost), while there is no evidence to date that supports “antigenic sin”. Pathogens evolve and mutate multiple times during one person’s life-span, if antigenic sin was how the immune system worked, quite simply, we’d all be dead.
But what this means is that B cells both take up residence and have some memory for where they first encountered the antigen and can evolve when they encounter a new version of the same antigen.
(Image Credit: Remembrance of Things Past: Long-Term B Cell Memory After Infection and Vaccination, Palm, AK. E. et al, Front. Immunol., 31 July 2019)
In summary, this is a very interesting finding and in case it holds up in follow up studies, it won’t hurt to have your COVID-19 booster shots given in the same arm and it may even help. As mentioned above, it is unclear how or if also having had COVID-19 would change these results. My best guess is that it would normalize the results between the two groups, but we really don’t know.
From the perspective of public health, it is possible that these results would hold true for other types of vaccination. This could have implications for the location of repeat dosing in childhood vaccines, influenza vaccines, and adult boosters for Tdap and MMR. I look forward to additional observational studies in this area to help establish best vaccination protocols.







This is a really interesting study that has not been looked at thoroughly previously. I agree with this assessment wholeheartedly and really enjoyed this analysis. Thank you so much!
Thank you for your analysis. I have Specific IGg Deficiency that requires me to have weekly self subcutaneous IGg infusions. I have had covid 4 x, and have had 6 Moderna shots/boosters. Going to give the same arm injection a try for the next round of shots! Will let you know!