Infectious Disease Roundup: 1/24/2025
An overview of infectious disease spread and outbreaks in the United States and globally
Special Note: As of now, the United States Health and Human Services (HHS) and its 13 departments remain in communications embargo. No new health data is being released, all research grant reviews as well as other internal operations have been halted or canceled. Data and notes in this roundup have been aggregated from local news agencies, the WHO, and state health departments.
Therefore, I may have missed important local notices from across the United States, please feel free to comment them or alert me to them so I can distribute information to my audience at large.
On LinkedIn today, the prior director of the NIH Monica Bertagnolli, MD (per NIH.gov her tenure ended January 17th, 2025. The current acting director is Matthew J. Memoli, MD, MS) wrote the following:
Per multiple news outlets, no comment has come from within the HHS or been made by current HHS employees.
Anonymous commenters on my social media pages have indicated that people inside the agencies are “terrified,” “do not know what is happening,” and many have said that communications inside the agencies have also been significantly disrupted.
Respiratory Virus Infections In The United States: The “Quad-demic”
Data from wastewaterscan.org, a project based out of Stanford University, California, shows that the United States currently has the highest levels of Influenza A and RSV in wastewater seen in the last 5 years.
Note: Beyond the four major virus sets shown above there are several other viruses in circulation that can cause symptoms ranging from a pesky cold to severe illness.
Since wastewater is a leading indicator, this means that we may not have reached the peak of respiratory virus infections for the 2024-25 season. The SARS-CoV-2 winter wave started later this year than previous years (as did RSV and influenza) perhaps due to a low number of highly similar variants in circulation (i.e. good cross-protective immunity) or perhaps infections were delayed by an unseasonably warm start to the fall and winter in the United States. Currently, most of the United States is experiencing extremely cold temperature, with snow in states like Florida, which are typically revered for their year-round beach weather. Most of these viruses are temperature sensitive (living longer when it is colder, but SARS-CoV-2 less so than others) which means that the recent cold snap may prolong the cold, flu, and COVID-19 season.
Recently in social media, I have noticed that people were surprised at how severe influenza can be. Perhaps the combination of low numbers of influenza infections in recent years and the anti-vaccine mantra of “it’s just the flu” lulled people into believing that influenza is an innocuous respiratory virus. It is not.
A bad influenza season in the United States can cause over 50,000 deaths (still at a lower rate than SARS-CoV-2) and lead to the hospitalization of hundreds of thousands of people (nearing a million in a bad year). Influenza also has its own version of post-acute sequelae (Long-Flu) in which people can have permanent damage or take months to recover from a severe infection.
Last influenza season, 200 children in the United States died from influenza infection, with deaths still being added to the tally as late as September 2023. The influenza vaccine is available to individuals ages 6 months and older. Because we do not have access to nationally aggregated data, I have combed local headlines and have found that since the CDC stopped reporting (16 children had died of influenza at the time), children have died in Mississippi and South Carolina. Part of the prior count included two pediatric deaths in Oregon and one in Wisconsin. The reason I am highlighting the pediatric deaths is that they are typically rare and indicate the severity of this flu season.
Currently, state new agencies in Minnesota are reporting overflowing emergency rooms, and UW Health in Wisconsin is reporting the highest levels of flu hospitalization in the last 3 years. Social media posts from frontline healthcare workers around the United States have indicated that this respiratory virus season is relentless. The same precautions used to prevent severe SARS-CoV-2 infection - hand washing, avoiding crowded spaces, mask wearing, and vaccination - all significantly reduce chances of severe influenza infection.
Norovirus has also been listed as part of the “quad-demic” (Influenza, SARS-CoV-2, RSV, and Norovirus). This virus has been found higher in wastewater this year compared to the past 5 years in the United States, but it has begun to trend downwards. Remember, a bleach-based cleaner should be used to kill Norovirus on surfaces and hand sanitizer is not effective at preventing a Norovirus infection.
(Source: wastewaterscan.org)
For information specific to your area, please visit your state health department’s website or wastewaterscan.org. If your state or local health department does not have up-to-date or timely data, I encourage you to write to them as well as your congressional representatives to encourage their support for public health.
Highly Pathogenic H5N1 influenza Update
An introduction to H5N1 influenza can be found here.
H5N1 influenza has been infecting wild birds and backyard flocks in Rhode Island and wild birds in Delaware, upstate New York, and West Philadelphia in the last couple of days. Large outbreaks in commercial poultry flocks across the United States from California and Nevada to Iowa, Georgia, Arkansas, Missouri, Illinois, and Maryland were reported this week in a CIRAP news brief. This has led to the culling of millions of birds causing a continued rise in the price of eggs, now up 36.8% from this time last year, as well as intermittent egg shortages. H5N1 has been found in wild birds and several other animals across the United States since 2022, but we are having a particularly bad outbreak of the disease this winter.
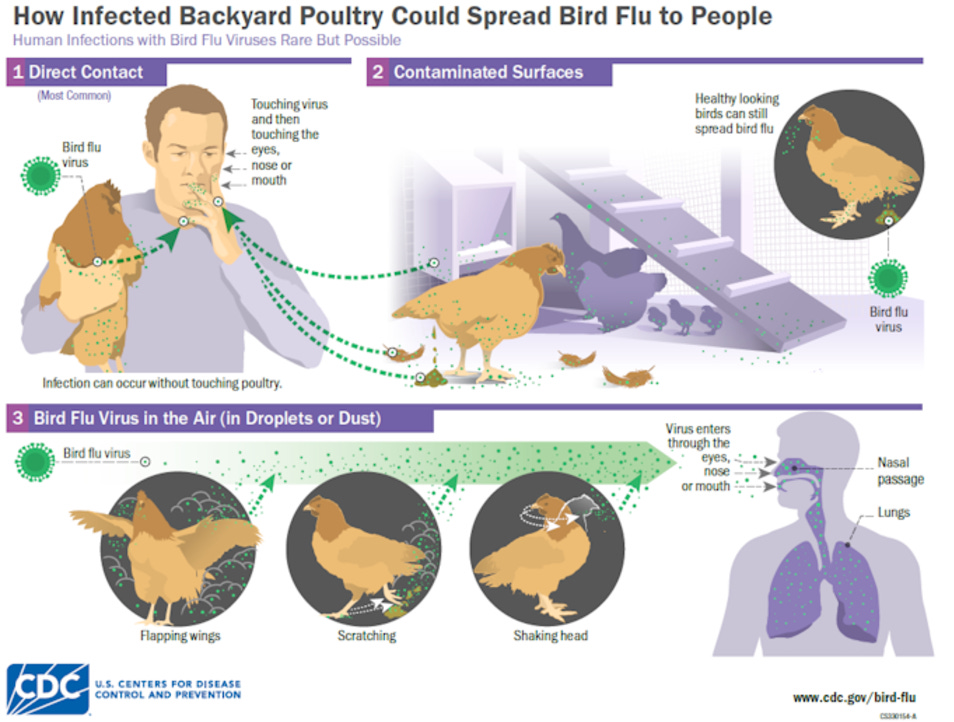
It is advised that people call their local wildlife or health department before handling sick or dying birds. If you must be in close contact with birds, wearing a high quality mask and disposable gloves or carefully washing your hand with soap and water can help reduce chances of becoming infected. Additionally, wearing goggles or protective eyewear may also help if there is prolonged contact with birds or bird droppings such as during cleaning of a chicken pen. Below is a graphic from the CDC that shows how bird flu can spread from birds to humans.
Also this week, the Minnesota Department of Health (MDH) issued a health advisory directing providers to test for H5N1 in patients hospitalized with Influenza A. This is in line with the Health Alert Network’s January 16th advisory encouraging increased subtyping. the first health advisory I have seen giving this directive. According to the department of health, this directive was in part triggered by the high levels of influenza and is in line with . This is also an acknowledgement of the need to ensure tracking and immediate response of any potential spill-over event where H5N1 may begin to spread person to person.
Human H5N1 cases are being tracked by World Health Organizations’ Global Influenza Surveillance and Response System (GISRS). Currently reported cases around the world look like this:
All human cases reported thus far have been found in the northern hemisphere. The vast majority of these cases have been reported in the United States.
This year’s flu vaccine may provide cross-protection and reduce symptoms for H5N1 when it becomes human to human spread. My prior substack detailing this can be found here.
Currently there are no reports of human to human spread.
Global Notes
Tanzania confirmed a new outbreak of Marburg virus disease on January 20th, 2025. The World Health Organization has sent both supplies and a team of scientists and medical professionals to help stop the outbreak. So far, the outbreak has a 90% case fatality rate. Local officials are concerned that the outbreak may spread rapidly as it is occurring in a high-traffic region of Tanzania that borders Burundi, Rwanda, and Uganda.
Respiratory virus illness is also high in China, with most hospitalizations and outpatient illness caused by influenza, RSV, and hMPV (Human metapneumovirus) across all age groups.
A global health success was announced yesterday as the country of Georgia has been certified as Malaria free. The decades-long effort supported by the WHO has eliminated malaria spread and committed resources to prevent re-emergence of the disease.
The WHO has issued an emergency appeal for funding in 2025. This is likely a direct result of the United States’ abrupt withdraw of support for the WHO. The vast majority of the world’s countries remain a part of the WHO (193 member states). The United States was a founding member of the WHO in 1948.
Looking Forward
I highly encourage everyone to stay up to date on their vaccines and if you have not had a booster for vaccines such as Tdap in the last 10 or so years it may be a good time to chat with your doctor regarding updating those as well. Often, an antibody titer test can be run to determine if you still have immunity. If you are traveling or plan to travel to a place where Polio still spreads, it is recommended that adults receive a polio booster. Also, be sure that children are up to date on their vaccinations.
As always, personal hygiene, mask wearing, and staying up to date with vaccines significantly reduces severity of illness.









Thank you! You have carried us through COVID and now continue to provide information during the federal pause (let’s hope it’s just that). I truly appreciate your efforts and knowledge.
Thank you!!! You are providing a little peace of mind in such stressful times